Delta Has Changed the Pandemic Risk Calculus
For the past year and a half, humans around the world have been asked to do something we’re pretty bad at, even in the best of circumstances: figure out what constitutes safety, and act accordingly. A well-understood risk doesn’t necessarily improve our thought processes, thanks to a host of cognitive biases and external pressures that pull some people away from the lowest-level danger and push others toward clear peril. In the United States, at least, the circumstances for making these decisions during the pandemic have been far from ideal, as millions of people have been yanked in either direction by misinformation or political stratification or financial necessity.
Vaccination was a reprieve from this calculus of personal danger, at least for a while—get vaccinated, get your family and friends vaccinated, get back to a far more normal version of life. To a certain extent, that logic holds: The vaccines are still doing a fantastic job preventing hospitalization and death from the coronavirus’s far-more-transmissible Delta variant. But as COVID-19 cases and hospitalizations have roared back, concerns about breakthrough cases among the vaccinated and increased transmissibility among kids have muddied a lot of people’s ability to gauge their own day-to-day risk, just as they’d begun to venture back out into the world and hug, eat, and laugh in the same airspace together again. In some ways, pandemic life is more confusing than ever.
What makes our current moment tricky is that pandemic risk has never been more highly variable, which means the list of things to consider about any given situation is longer and has fewer hard-and-fast rules. Vaccinated people are still far safer than they’ve been for most of the past year and a half, and the unvaccinated are in even more danger than they were in March 2020. The Delta variant is, in some respects, a whole new ball game. What rules are we playing by now?
Delta behaves differently from those that came before it in key ways: It spreads between people far more effectively, it seems more likely to cause a contagious “breakthrough infection” in vaccinated people, and it appears to spread more readily and lead to symptomatic disease more often among kids too young to be vaccinated. Whether Delta causes more virulent disease is, for now, an open question. We’ll get to more open questions shortly.
[Read: How the pandemic now ends]
Because of these differences, there are two categories of things you should consider when you contemplate booking a vacation or responding to a wedding invite. The first is what you might reasonably know about your situation and the event at hand. “It’s your vaccination, and then the vaccination levels of people around you, and then the disease rates happening around you,” Tara Kirk Sell, a researcher who studies risk communication at the Johns Hopkins Center for Health Security, told me. “Do you have kids or not? Are they going to school?” All of these types of questions, she said, help paint a picture of the potential danger you might represent to unprotected people around you, should you get sick. The less likely you are to be exposed and the fewer unvaccinated or immunocompromised people you could conceivably infect, the more confident you should feel.
Assessing risk pre-vaccination was often bleak, but at least the variables at play were somewhat limited: ventilation, masks, crowds, local spread. Now the number of additional, usually hyper-specific questions that people must ask themselves is itself a barrier to good decision making, says Jennifer Taber, a psychologist at Kent State University who studies health risk assessment. “When people feel like things are uncertain, they engage in avoidance,” Taber told me. That can manifest in disparate ways. An unwillingness to acknowledge that many new things are safe for the average vaccinated person is avoidance. So is a refusal to continue taking even minor precautions for the benefit of others.
All of this is made worse given that accurate answers to risk-related questions can be frustrating to gather and difficult to parse, especially in places where local governments limit data collection, and where admitting to being vaccinated can be social apostasy. “There are so many things that make it harder, and not a lot of things that make it easier right now,” Taber said. “Even within the context of good information, there’s so much uncertainty that it makes it really hard for people to make really well-informed decisions.”
That brings us to the second, murkier category of information to consider when gauging the safety of a situation: What do we actually know about the Delta variant and the risks it presents? The situation is, unfortunately, evolving. Because the United States is testing at only a fraction of the rate of countries such as Israel and the U.K.—stop me if this is giving you flashbacks to the spring of 2020—the frustrating reality is that we just do not have a reliable picture of how much infection is currently happening here. When you don’t have an accurate denominator on which to base things such as rate of breakthrough, hospitalization, or death, you have a pretty useless fraction. (Unfortunately, for similar reasons, we are also short on accurate numerators—the CDC is not tracking things like breakthrough infections, and state-level data are sparse.)
[Read: The messiest phase of the pandemic yet]
Unvaccinated people tend to be clustered both geographically and socially in the United States, and so national or even state-level rates of vaccination are not terribly useful in understanding personal risk. The catastrophic spikes in infection currently devastating places with low vaccination rates, such as southern Louisiana and southeastern Missouri, change how even vaccinated people in those places should think about socializing or traveling, relative to their counterparts in places with high community buy-in on vaccines. Because they are far more likely to be exposed to the virus than someone living in, say, Vermont or Maine, the knock-on effect is a far greater likelihood of spreading the infection to others. And as Florida’s current outbreak makes clear, even middle-of-the-road statewide vaccination rates will not be enough to dampen Delta’s spread on their own.
These gaps in information and state-by-state discrepancies make any sort of risk generalizations difficult, if not counterproductive. What we do know is that vaccination remains the best way to stay healthy, by far: According to a survey of hospitals from ABC News, 94 percent of COVID-19 patients in ICUs at the end of July were unvaccinated, and most of the rest had health problems that likely contributed to decreased vaccine effectiveness. Young, healthy vaccinated people who are working in person or socializing in crowds should take precautions around elderly or immunocompromised friends and family, even if they are also vaccinated, but overall, vaccinated people still can feel quite confident in their personal safety.
How the vaccines are doing against any level of infection is less clear. The most recent and comprehensive data available—from the U.K.—suggest that current vaccine regimens are somewhat less effective against Delta than against previous strains of the virus, but the difference isn’t enormous. If that information feels at odds with reports you’ve heard about breakthrough infections in the U.S., it isn’t necessarily—uncontrolled spread of a highly infectious disease means that even relatively uncommon events are going to happen in pretty large numbers.
Speaking of breakthroughs: One thing that needs to be accounted for is the potential of infecting others if you become sick, even after getting vaccinated. A few weeks ago, the CDC raised eyebrows by estimating that vaccinated people who manage to get infected by Delta may produce the same amount of virus in their nose as unvaccinated, Delta-infected people do—an unexpected sign that vaccinated people could be equally contagious when infected. But the agency’s analysis was based on specific and fairly extreme circumstances: an outbreak in Provincetown, Massachusetts, among a mostly vaccinated group during a week of festivities in which people crowded into old, poorly ventilated buildings. A large analysis of Delta transmission in the U.K. found that vaccinated people carry, on average, lower levels of virus in their nose, which suggests less ability to transmit the virus; a recent study from Singapore found that vaccinated patients were able to clear the virus much faster, shortening the number of days during which they might be contagious. (Although no data are available quite yet, the efficiency with which vaccinated people clear the virus is also thought to make the sometimes severe post-viral COVID-19 symptoms commonly known as long COVID considerably less likely, by preventing the illness from settling in the lungs.)
What must be acknowledged now, a year and a half into the pandemic, is that COVID-19 is not the only risk that people need to balance. Forgoing regular socializing, routine medical checkups, and in-person schooling might be worthwhile in the short term, but abstaining from all of those things in perpetuity comes with its own dangers. “What we’ve given up is not nothing,” Kirk Sell told me. “Something that has been lost in the past year and a half are the trade-offs, and the introduction of readily available and highly effective vaccines and some people’s refusal to get them just makes all of this internal math so much trickier.” As someone who studies risk communication, she said, she hates the phrase an abundance of caution. If you find yourself determining that things you want to do are pretty low risk and still shy away from them, you’re likely cutting yourself off from opportunities that may provide significant health benefits: getting out to exercise, resuming regular social relationships with vaccinated friends and family.
Kirk Sell uses her own decision calculus as an example of what those kinds of evaluations might look like: She thinks it’s very important for her kids to have school in person, even though they are too young to be vaccinated, but she is also actively lobbying the school to implement ways to make that safer, such as enhanced ventilation and filtration. For parents whose kids did relatively well in Zoom school or whose community is in the middle of a serious outbreak, she says, the best conclusion might be a different one, and it might change for any parent as the school year progresses and local case rates go up and down.
[Read: The coronavirus is here forever. This is how we live with it.]
Try thinking about precautions in non-pandemic terms, Kirk Sell advises. Every day, people follow safety rules that might not be personally necessary for them, but that also aren’t onerous enough to be harmful—doing so is simply part of living in a society in which you share norms and risk with those around you. “I can swim, but when I go out kayaking, I still wear a life jacket, because it’s required as a general safety approach,” she explained. “Just because you are safe doesn’t mean you don’t have any rules to follow anymore.” This is, perhaps, somewhat understating it: Before Kirk Sell was a scholar, she was an Olympic-medalist swimmer who held the world record in the 100-meter breaststroke. There are few people on Earth at less personal risk from tipping out of a kayak. So, yes, you can probably find it within yourself to continue to wear a mask at the grocery store if the infection rate is growing in your area. You probably do other stuff on that same logic all the time.
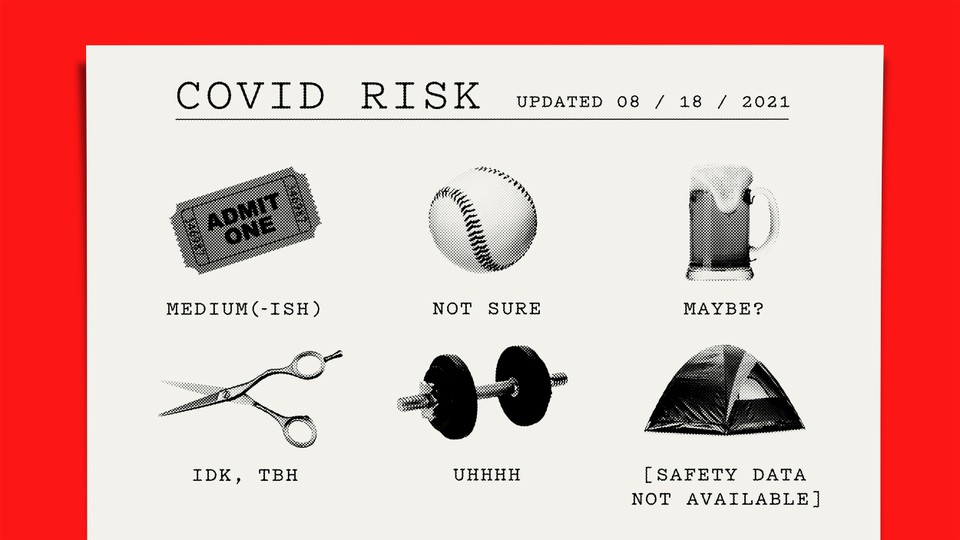
If you have read all this hoping to get some solid answers on what you should be doing and now feel like it would have been easier for me to publish, say, a shrugging emoji, I sympathize. It can be difficult to feel like you’re doing the right thing when what that means is so different from person to person, depending on their particular circumstances. People frequently use the behavior of those around them to guide their own understanding of risk, Taber told me, and the fact that everyone around you now has a whole host of personal circumstances to consider when making their own decisions can short-circuit our ability to do that as confidently as we might have a year ago.
Americans will likely be riding this roller coaster of risk assessment for some time. Periods of confusion are natural as we learn what waves of the Delta variant under the country’s modest-at-best safety protocols look like, and we’ve yet to see how swiftly the next wave can be expected after one ends. People are tired of good behavior, and they’re tired of self-abnegating to protect others whom they perceive as refusing to protect themselves, even if that’s not an accurate understanding of why many people have yet to be vaccinated. Right now, the best that most people can do is continue to control whichever straightforward variables they can—get vaccinated, sit outside when possible, choose places that require proof of vaccination over those that don’t, avoid visiting Grandma or your cousin’s new baby the week after attending an indoor concert with a thousand screaming people, get a test if your throat is sore. The situation we’re all in is extremely complicated, but the best ways to keep yourself and others safe still aren’t.